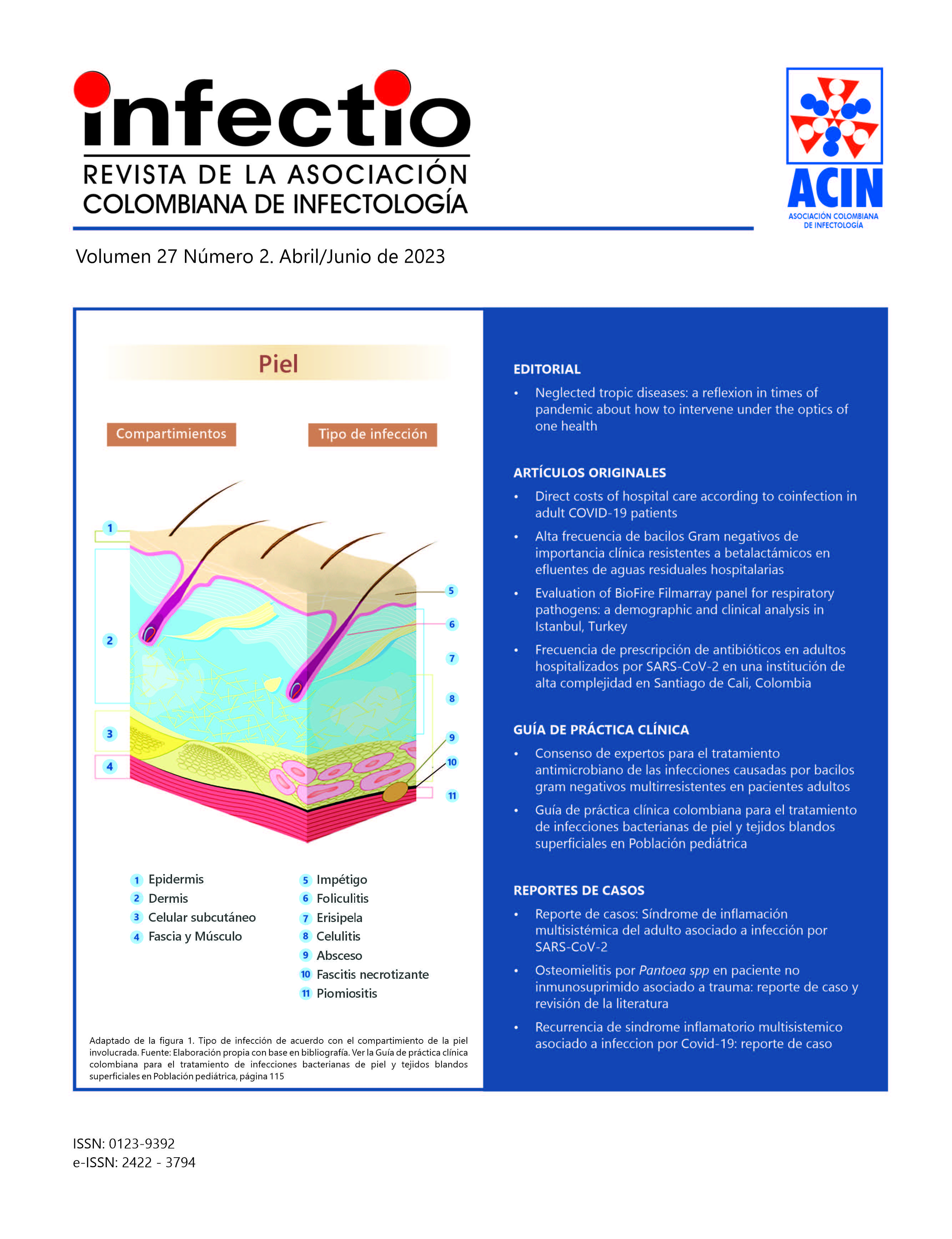
Guía de práctica clínica colombiana para el tratamiento de infecciones bacterianas de piel y tejidos blandos superficiales en Población pediátrica
Contenido principal del artículo
Resumen
En el año 2019 se publicó la guía de práctica clínica para el diagnóstico y manejo de las infecciones de piel y tejidos blandos en Colombia. Dicha guía excluía a la población pediátrica por sus consideraciones especiales. Teniendo en cuenta que estas infecciones representan un motivo de consulta frecuente en pediatría y que la emergencia del Staphylococcus aureus resistente a meticilina generan la necesidad de actualizar conocimientos y estrategias para el manejo de las infecciones de piel y tejidos blandos superficiales, se presenta esta guía de práctica clínica que da respuesta basada en la evidencia a 12 preguntas. Dicha evidencia fue adaptada y graduada bajo el sistema GRADE posterior a un proceso de adaptación de tres guías publicadas. Adicionalmente, se realizó una actualización de la evidencia científica bajo una búsqueda sistemática. Por último, se realizó un consenso de expertos para la evaluación de las potenciales barreras para la implementación de las recomendaciones en el contexto local.
Detalles del artículo
Citas
Galli L., Venturini E., Bassi A., Gattinara GC., Chiappini E., De C., et al. Common Community-acquired Bacterial Skin and Soft-tissue Infections in Children : an Intersociety Consensus on Impetigo , Abscess , and Cellulitis Treatment. Clinical Therapeutics. 2019;41(3):532-51, doi:10.1016/j.clinthera.2019.01.010.
Sociedad Argentina de Pediatría, Moyano M., Peuchot A., Giachetti AC., Moreno R., Cancellara A., et al. Infecciones de piel y partes blandas en pediatría: consenso sobre diagnóstico y tratamiento. Arch Argent Pediatr. 2014;112(1):e96-102, doi: 10.5546/aap.2014.e96.
Valderrama Beltran S., Cortés JA., Caro MA., Cely Andrade L., Osorio Pinzón JV., Gualtero SM., et al. Guía de práctica clínica para el diagnóstico y manejo de las infecciones de piel y tejidos blandos en Colombia. Infectio. 2019;23(4):318-46, doi: http://dx.doi.org/10.22354/in.v23i4.805.
Conejo Fernández A., Martínez Roig A., Ramírez Balza O., Álvez González F., Hernández Hernández A., Baquero Artigao F., et al. Documento de consenso SEIP-AEPap-SEPEAP sobre la etiología, el diagnóstico y el tratamiento de las infecciones cutáneas micóticas de manejo ambulatorio. Pediatria de Atencion Primaria. 2016;18(72):e149-72, doi:10.1016/j.anpedi.2015.01.002.
Weiner L., Webb A., Limbago B., Dudeck M., Patel J., Kallen A., et al. Antimicrobial-Resistant Pathogens Associated With Healthcare- Associated Infections: Summary of Data Reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2011–2014. Physiology & behavior. 2019;176(3):139-48, doi:10.1016/j.physbeh.2017.03.040.
Grupo para el control de la resistencia bacteriana de Bogotá (GREBO) Resultados de la vigilancia de la resistencia bacteriana. Año 2018: Componente pediátrico y adulto. Bogotá, Colombia: GREBO; 2019.
Shankar N., Soe P mar., Tam CC. Prevalence and risk of acquisition of methicillin-resistant Staphylococcus aureus among households: A systematic review. International Journal of Infectious Diseases. 2020;92:105-13, doi: 10.1016/j.ijid.2020.01.008.
Wong JWH., Ip M., Tang A., Wei VWI., Wong SYS., Riley S., et al. Prevalence and risk factors of community-associated methicillin-resistant staphylococcus aureus carriage in asia-pacific region from 2000 to 2016: A systematic review and meta-analysis. Clinical Epidemiology. 2018;10:1489-501, doi: 10.2147/CLEP.S160595.
Droz N., Hsia Y., Ellis S., Dramowski A., Sharland M., Basmaci R. Bacterial pathogens and resistance causing community acquired paediatric bloodstream infections in low- And middle-income countries: A systematic review and meta-analysis. Antimicrobial Resistance and Infection Control. 2019;8(1):1-12, doi: 10.1186/s13756-019-0673-5.
Orjuela Mateus L., Quijana Muñoz CL., Gutierrez IF. Caracterización de la infección por Staphylococcus aureus en población pediátrica en infantes. Tesis para obtener el título de pediatra, Universidad del Rosario, Bogotá D.C., Colombia, 2016.
Reyes J., Rincón S., Díaz L., Panesso D., Contreras GA., Zurita J., et al. Dissemination of Methicillin-Resistant Staphylococcus aureus USA300 Sequence Type 8 Lineage in Latin America. Clinical Infectious Diseases. 2009;49(12):1861-77, doi: 10.1086/648426.
Escobar-Perez J., Castro B., Marquez-Ortiz R., Gaines S., Chavarro Portillo B., Moreno J., et al. Methicillin-sensitive Staphylococcus aureus isolates related to USA300 clone: Origin of community-genotype MRSA in Colombia? Biomedica : revista del Instituto Nacional de Salud. 2014;34(Suppl 1):124-36, doi: 10.1590/S0120-41572014000500015.
Zhong A., Caro MA., Valderrama-Beltrán. Registro multicéntrico de infecciones de piel y tejidos blandos en pacientes hospitalizados 2009- 2014 en Colombia. Tesis para optar por el título de especialista en medicina interna, Pontificia Universidad Javeriana, Bogotá D.C., Colombia, 2014.
Valderrama S., Moreno CAA., Gualtero S., Osorio J., Rodriguez J., Quintero CG., et al. Multicenter Study of Skin and Soft Tissue Infections Complicated in Hospitalized Patients 2009–2014 in Colombia. Open Forum Infectious Diseases. 2015;2(suppl_1):1532, doi: 10.1093/ofid/ofv133.1085.
Valderrama-Beltrán S., Gualtero S., Álvarez-Moreno C., Gil F., Ruiz AJ., Rodríguez JY., et al. Risk factors associated with methicillin-resistant Staphylococcus aureus skin and soft tissue infections in hospitalized patients in Colombia. Int J Infect Dis. 2019;87:60-6, doi: 10.1016/j.ijid.2019.07.007.
Collazos Marín LF., Estupiñan Arciniegas G., Chavez Vivas M. Characterization of Staphylococcus aureus Isolates That Colonize Medical Students in a Hospital of the City of Cali, Colombia. International Journal of Microbiology. 2015;2015(Article ID 358489):1-6, doi:10.1155/2015/358489.
Sánchez Y., Urbano EX., González FJ., Ferrebuz AJ. Caracterización fenotípica de cepas de Staphylococcus aureus productoras de Beta-lactamasas y resistente a la meticilina. Revista Investig Salud Univ Boyacá. 2018;5(1):125-43, doi: 10.24267/23897325.302.
Montes O., Milanés R., Alvarez A., Coronado S., Reyes N. Características moleculares y susceptibilidad a antibióticos de cepas de Staphylococcus aureus colonizantes de pacientes con patologías nasales procedentes de Cartagena (Colombia), 2015: estudio observacional. archmed. 2015;15(2):226-40, doi: 10.30554/archmed.15.2.743.2015.
Castro-Orozco R., Villafañe-Ferrer LM., álvarez-Rivera E., Martínez De Arco M., Rambaut-Donado CL., Vitola-Heins GV. Staphylococcus aureus meticilino resistente en niños escolares de Cartagena. Revista de Salud Pública. 2010;12(3):454-63, doi: 10.1590/S0124-00642010000300011.
Figueroa-Vargas A., Arteaga-Jiménez ME., Aguirre JA., Martínez SY., Solano-Vivas VE., Delgado-Noguera M. Infecciones por Estafilococo aureus meticilinoresistente adquirido en la comunidad en Popayán, Colombia. Revista de la Facultad de Ciencias de la Salud Universidad del Cauca. 2010;12(4):9-13.
Sosa Ávila LM., Machuca Pérez MA., Sosa Ávila CA., González Rugeles CI. Infecciones por Staphylococcus aureus meticilino resistente en niños en Bucaramanga Colombia. Revista de la Universidad Industrial de Santander Salud. 2010;42(3):248-55.
Castaño-Jaramillo LM., Beltrán-Arroyave C., Santander-Peláez LC., Vélez- Escobar AM., Garcés-Samudio CG., Trujillo-Honeysberg M. Características clínicas y microbiológicas de las infecciones de piel y tejidos blandos por Staphylococcus aureus en niños de un hospital en Medellín durante los años 2013 a 2015. Rev chil infectol. 2017;34(5):487-90, doi: 10.4067/S0716-10182017000500487.
Ricardo-Caldera DM., Buelvas-Doria FA., Escobar-Pérez JA., Tovar-Acero C. Colonización y factores de virulencia de Staphylococcus aureus resistente a meticilina en una población infantil de Montería. Iatreia. 2015;28(3):259- 68, doi: 10.17533/udea.iatreia.v28n3a04.
Pérez N., Pavas N., Isabel Rodríguez E. Resistencia de Staphylococcus aureus a los antibióticos en un hospital de la orinoquia colombiana. Infectio. 2010;14(3):167-73, doi: 10.1016/S01239392(10)70108-9.
Sánchez Lerma L., Pavas Escobar NC., Rojas Gulloso A., Pérez Gutiérrez N. Infecciones por Staphylococcus aureus resistente a la meticilina adquirido en la comunidad en pacientes de Villavicencio, Colombia. Revista Cubana de Medicina Tropical. 2016;68(1):40-50.
Schunemann HJ., Wiercioch W., Brozek J., Etxeandia-Ikobaltzeta I., Mustafa RA., Manja V., et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. Journal of Clinical Epidemiology. 2017;81:101-10, doi: 10.1016/j.jclinepi.2016.09.009.
Schunemann HJ., Mustafa R., Brozek J., Santesso N., Alonso-Coello P., Guyatt G., et al. GRADE Guidelines: 16. GRADE evidence to decisión frameworks for tests in clinical practice and public health. J Clin Epidemiol. 2016;76:89-98, doi: 10.1016/j.jclinepi.2016.01.032.
Brouwers MC., Kerkvliet K., Spithoff K., AGREE Next Steps Consortium The AGREE Reporting Checklist: a tool to improve reporting of clinical practice guidelines. BMJ. 2016:i1152, doi: 10.1136/bmj.i1152.
Stevens DL., Bisno AL., Chambers HF., Dellinger EP., Goldstein EJC., Gorbach SL., et al. Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2014;59(2):e10-52, doi:10.1093/cid/ciu296.
Kwak YG., Choi S-H., Kim T., Park SY., Seo S-H., Kim MB., et al. Clinical Guidelines for the Antibiotic Treatment for Community-Acquired Skin and Soft Tissue Infection. Infect Chemother. 2017;49(4):301, doi: 10.3947/ ic.2017.49.4.301.
Somerville J. Critical Factors Affecting the Assessment of Student Learning Outcomes: A Delphi Study of the Opinions of Community College Personnel. Journal of Applied Research in the Community College. 2008;15(2):109-19.
Cabero Almenara J., Infante Moro A. Empleo del método Delphi y su empleo en la investigación en comunicación y educación. Edutec Revista Electrónica de Tecnología Educativa. 2014;(48):1-16, doi: 10.21556/edutec.2014.48.187.
Varela-Ruiz M., Díaz-Bravo L., García-Durán R. Descripción y usos del método Delphi en investigaciones del área de la salud. Investigación en educación médica. 2012;1(2):90-5.
Guyatt GH., Oxman AD., Vist GE., Kunz R., Falck-Ytter Y., Alonso-Coello P., et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924-6, doi: 10.1136/bmj.39489.470347.AD.
Koning S., van der Sande R., Verhagen AP., van Suijlekom-Smit LW., Morris AD., Butler CC., et al. Interventions for impetigo. Cochrane Database of Systematic Reviews. 2012:1-135, doi: 10.1002/14651858.CD003261.pub3.
Long SS., Brady MT., Jackson MA., Kimberlin DW. Red Book 2018: Report of the Committee on Infectious Diseases. Elk Grove Village: American Academy of Pediatrics; 2018.
Regamey C. Cefazolin vs Cephalothin and Cephaloridine: A Comparison of Their Clinical Pharmacology. Arch Intern Med. 1974;133(3):407-10, doi: 10.1001/archinte.1974.00320150081009.
Dillon HC. Treatment of staphylococcal skin infections: a comparison of cephalexin and dicloxacillin. J Am Acad Dermatol. 1983;8(2):177-81, doi:10.1016/s0190-9622(83)70020-4.
Harrison CJ., Marks MI., Welch DF., Sharma BB., Baker D., Dice J. A multicenter comparison of related pharmacologic features of cephalexin and dicloxacillin given for two months to young children with cystic fibrosis. Pediatr Pharmacol (New York). 1985;5(1):7-16.
Bayhan GI., Akbayram S., Ozaydin Yavuz G., Oner AF. Cutaneous side effects of doxycycline: a pediatric case series. Cutaneous and Ocular Toxicology. 2017;36(2):140-4, doi: 10.1080/15569527.2016.1195840.
Nelson, Barnett ED., Bradley JS. Nelson. Terapia antimicrobiana en pediatría. Barcelona: Elsevier; 2017.
Bangert S., Levy M., Hebert AA. Bacterial Resistance and Impetigo Treatment Trends: A Review. Pediatric Dermatology. 2012;29(3):243-8, doi: https://doi.org/10.1111/j.1525-1470.2011.01700.x.
Hartman-Adams H., Banvard C., Juckett G. Impetigo: diagnosis and treatment. Am Fam Physician. 2014;90(4):229-35.
Scheinfeld NS. Is blistering distal dactylitis a variant of bullous impetigo? Clinical and Experimental Dermatology. 2007;32(3):314-6, doi: https://doi.org/10.1111/j.1365-2230.2007.02379.x.
Chamny S., Miron D., Lumelsky N., Shalev H., Gazal E., Keynan R., et al. Topical Minocycline Foam for the Treatment of Impetigo in Children: Results of a Randomized, Double-Blind, Phase 2 Study. J Drugs Dermatol. 2016;15(10):1238-43.
García E., Halpert E., Borrero E., Ibañez M., Chaparro P., Molina J., et al. Prevalence of skin diseases in children 1 to 6 years old in the city of Bogota, Colombia. World Allergy Organization Journal. 2020;13(12):100484, doi:10.1016/j.waojou.2020.100484.
Alcaraz G., Bernal C., Cornejo W., Figueroa N., Múnera M. Estado nutricional y condiciones de vida de los niños menores de cinco años del área urbana del municipio de Turbo, Antioquia, Colombia, 2004. Biomédica. 2008;28(1):87-96, doi: 10.7705/biomedica.v28i1.111.
Nuñez L F., Zarante IM., Bernal V JE. Estado de Salud infantil en las comunidades indígenas, afrocolombianas y aisladas en Colombia. Medicina. 2002;24(1):27-42.
Tanus T., Scangarella-Oman NE., Dalessandro M., Li G., Breton JJ., Tomayko JF. A Randomized, Double-blind, Comparative Study to Assess the Safety and Efficacy of Topical Retapamulin Ointment 1% Versus Oral Linezolid in the Treatment of Secondarily Infected Traumatic Lesions and Impetigo Due to Methicillin-Resistant Staphylococcus aureus. Advances in Skin & Wound Care. 2014;27(12):548-59, doi: 10.1097/01.ASW.0000456631.20389.ae.
Mundy LM., Sampson T., Logie JW. Retapamulin Prescriptions and Monitored Off-Label Use. Pediatr Drugs. 2014;16(4):331-6, doi: 10.1007/s40272-014-0077-1.
McNeil JC., Hulten KG., Kaplan SL., Mason EO. Decreased Susceptibilities to Retapamulin, Mupirocin, and Chlorhexidine among Staphylococcus aureus Isolates Causing Skin and Soft Tissue Infections in Otherwise Healthy Children. Antimicrobial Agents and Chemotherapy. 2014;58(5):2878-83, doi: 10.1128/AAC.02707-13.
Iovino SM., Krantz KD., Blanco DM., Fernández JA., Ocampo N., Najafi A., et al. NVC-422 topical gel for the treatment of impetigo. Int J Clin Exp Pathol. 2011;4(6):587-95.
Gropper S., Cepero AL., Santos B., Kruger D. Systemic bioavailability and safety of twice-daily topical ozenoxacin 1% cream in adults and children with impetigo. Future Microbiology. 2014;9(8s):S33-40, doi: 10.2217/fmb.14.85.
Bowen AC., Tong SYC., Andrews RM., O’Meara IM., McDonald MI., Chatfield MD., et al. Short-course oral co-trimoxazole versus intramuscular benzathine benzylpenicillin for impetigo in a highly endemic region: an open-label, randomised, controlled, non-inferiority trial. Lancet. 2014;384(9960):2132-40, doi: 10.1016/S0140-6736(14)60841-2.
Wasserzug O., Valinsky L., Klement E., Bar Zeev Y., Davidovitch N., Orr N., et al. A Cluster of Ecthyma Outbreaks Caused by a Single Clone of Invasive and Highly Infective Streptococcus pyogenes. CLIN INFECT DIS. 2009;48(9):1213-9, doi: 10.1086/597770.
Raff AB., Kroshinsky D. Cellulitis: A Review. JAMA. 2016;316(3):325-37, doi: 10.1001/jama.2016.8825.
Eells SJ., Chira S., David CG., Craft N., Miller LG. Non-suppurative cellulitis: risk factors and its association with Staphylococcus aureus colonization in an area of endemic community-associated methicillin-resistant S. aureus infections. Epidemiology & Infection. 2011;139(4):606-12, doi: 10.1017/S0950268810001408.
Swartz MN. Clinical practice. Cellulitis. N Engl J Med. 2004;350(9):904-12, doi: 10.1056/NEJMcp031807.
Duvanel T., Auckenthaler R., Rohner P., Harms M., Saurat JH. Quantitative cultures of biopsy specimens from cutaneous cellulitis. Arch Intern Med. 1989;149(2):293-6.
Kwak YG., Kim NJ., Choi S-H., Choi S-H., Chung J-W., Choo EJ., et al. Clinical Characteristics and Organisms Causing Erysipelas and Cellulitis. Infection & Chemotherapy. 2012;44(2):45-50, doi: 10.3947/ic.2012.44.2.45.
Park SY., Kim T., Choi S H., Jung J., Yu SN., Hong H-L., et al. Impact of health care-associated community-onset cellulitis in Korea: a multicenter study. Eur J Clin Microbiol Infect Dis. 2019;38(3):545-52, doi: 10.1007/s10096-018-03456-0.
Malone JR., Durica SR., Thompson DM., Bogie A., Naifeh M. Blood cultures in the evaluation of uncomplicated skin and soft tissue infections. Pediatrics. 2013;132(3):454-9, doi: 10.1542/peds.2013-1384.
Trenchs V., Hernandez-Bou S., Bianchi C., Arnan M., Gene A., Luaces C. Blood Cultures Are Not Useful in the Evaluation of Children with Uncomplicated Superficial Skin and Soft Tissue Infections. Pediatr Infect Dis J. 2015;34(9):924-7, doi: 10.1097/INF.0000000000000768.
Elliott DJ., Zaoutis TE., Troxel AB., Loh A., Keren R. Empiric antimicrobial therapy for pediatric skin and soft-tissue infections in the era of methicillin-resistant Staphylococcus aureus. Pediatrics. 2009;123(6):e959-966, doi: 10.1542/peds.2008-2428.
Pallin DJ., Binder WD., Allen MB., Lederman M., Parmar S., Filbin MR., et al. Clinical trial: comparative effectiveness of cephalexin plus trimethoprimsulfamethoxazole versus cephalexin alone for treatment of uncomplicated cellulitis: a randomized controlled trial. Clin Infect Dis. 2013;56(12):1754-62, doi: 10.1093/cid/cit122.
Moran GJ., Krishnadasan A., Mower WR., Abrahamian FM., LoVecchio F., Steele MT., et al. Effect of Cephalexin Plus Trimethoprim-Sulfamethoxazole vs Cephalexin Alone on Clinical Cure of Uncomplicated Cellulitis: A Randomized Clinical Trial. JAMA. 2017;317(20):2088-96, doi: 10.1001/jama.2017.5653.
Jeng A., Beheshti M., Li J., Nathan R. The role of beta-hemolytic streptococci in causing diffuse, nonculturable cellulitis: a prospective investigation. Medicine (Baltimore). 2010;89(4):217-26, doi: 10.1097/MD.0b013e3181e8d635.
McMullan BJ., Andresen D., Blyth CC., Avent ML., Bowen AC., Britton PN., et al. Antibiotic duration and timing of the switch from intravenous to oral route for bacterial infections in children: systematic review and guidelines. Lancet Infect Dis. 2016;16(8):e139-152, doi: 10.1016/S1473-3099(16)30024-X.
Korczowski B., Antadze T., Giorgobiani M., Stryjewski ME., Jandourek A., Smith A., et al. A Multicenter, Randomized, Observer-blinded, Activecontrolled Study to Evaluate the Safety and Efficacy of Ceftaroline Versus Comparator in Pediatric Patients With Acute Bacterial Skin and Skin Structure Infection. Pediatr Infect Dis J. 2016;35(8):e239-247, doi: 10.1097/INF.0000000000001191.
Rosanova MT., Aguilar PS., Sberna N., Lede R. Efficacy and safety of ceftaroline: systematic review and meta-analysis. Ther Adv Infect Dis. 2019;6:2049936118808655, doi: 10.1177/2049936118808655.
Bradley J., Glasser C., Patino H., Arnold SR., Arrieta A., Congeni B., et al. Daptomycin for Complicated Skin Infections: A Randomized Trial. Pediatrics. 2017;139(3):e20162477, doi: 10.1542/peds.2016-2477.
Oh DH., Kim JJ., Kim J., Seong H., Lee SJ., Kim YC., et al. Comparison of the efficacy of nafcillin and glycopeptides as definitive therapy for patients with methicillin-susceptible Staphylococcus aureus bacteremia: a retrospective cohort study. BMC Infect Dis. 2018;18(1):60, doi: 10.1186/s12879-018-2978-z.
Kim S H., Kim K H., Kim H B., Kim N J., Kim E C., Oh M., et al. Outcome of vancomycin treatment in patients with methicillin-susceptible Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2008;52(1):192-7, doi: 10.1128/AAC.00700-07.
Schweizer ML., Furuno JP., Harris AD., Johnson JK., Shardell MD., McGregor JC., et al. Comparative effectiveness of nafcillin or cefazolin versus vancomycin in methicillin-susceptible Staphylococcus aureus bacteremia. BMC Infect Dis. 2011;11:279, doi: 10.1186/1471-2334-11-279.
Davis JS., Sud A., O Sullivan MVN., Robinson JO., Ferguson PE., Foo H., et al. Combination of Vancomycin and Beta-Lactam Therapy for Methicillin- Resistant Staphylococcus aureus Bacteremia: A Pilot Multicenter Randomized Controlled Trial. Clin Infect Dis. 2016;62(2):173-80, doi:10.1093/cid/civ808.
Fox PM., Lampen RJ., Stumpf KS., Archer GL., Climo MW. Successful Therapy of Experimental Endocarditis Caused by Vancomycin-Resistant Staphylococcus aureus with a Combination of Vancomycin and Beta-Lactam Antibiotics. Antimicrob Agents Chemother. 2006;50(9):2951-6, doi:10.1128/AAC.00232-06.
Tabuchi F., Matsumoto Y., Ishii M., Tatsuno K., Okazaki M., Sato T., et al. Synergistic effects of vancomycin and beta-lactams against vancomycin highly resistant Staphylococcus aureus. J Antibiot (Tokyo). 2017;70(6):771- 4, doi: 10.1038/ja.2017.7.
Guillamet CV., Kollef MH. How to stratify patients at risk for resistant bugs in skin and soft tissue infections? Curr Opin Infect Dis. 2016;29(2):116-23, doi: 10.1097/QCO.0000000000000244.
Miller LG., Daum RS., Creech CB., Young D., Downing MD., Eells SJ., et al. Clindamycin versus Trimethoprim–Sulfamethoxazole for Uncomplicated Skin Infections. New England Journal of Medicine. 2015;372(12):1093-103, doi: 10.1056/NEJMoa1403789.
Talan DA., Mower WR., Krishnadasan A., Abrahamian FM., Lovecchio F., Karras DJ., et al. Trimethoprim–Sulfamethoxazole versus Placebo for Uncomplicated Skin Abscess. New England Journal of Medicine. 2016;374(9):823-32, doi: 10.1056/NEJMoa1507476.
Holmes L., Ma C., Qiao H., Drabik C., Hurley C., Jones D., et al. Trimethoprim-Sulfamethoxazole Therapy Reduces Failure and Recurrence in Methicillin-Resistant Staphylococcus aureus Skin Abscesses after Surgical Drainage. The Journal of Pediatrics. 2016;169:128-134.e1, doi:10.1016/j.jpeds.2015.10.044.
Moore SJ., O’Leary ST., Caldwell B., Knepper BC., Pawlowski SW., Burman WJ., et al. Clinical characteristics and antibiotic utilization in pediatric patients hospitalized with acute bacterial skin and skin structure infection. Pediatr Infect Dis J. 2014;33(8):825-8, doi: 10.1097/INF.0000000000000304.
Sunderkotter C., Becker K. Frequent bacterial skin and soft tissue infections: diagnostic signs and treatment. J Dtsch Dermatol Ges. 2015;13(6):501-24; quiz 525-6, doi: 10.1111/ddg.12721.
Barbic D., Chenkin J., Cho DD., Jelic T., Scheuermeyer FX. In patients presenting to the emergency department with skin and soft tissue infections what is the diagnostic accuracy of point-of-care ultrasonography for the diagnosis of abscess compared to the current standard of care? A systematic review and meta-analysis. BMJ Open. 2017;7(1):e013688, doi: 10.1136/bmjopen-2016-013688.
Singer AJ., Thode HC. Systemic antibiotics after incision and drainage of simple abscesses: a meta-analysis. Emerg Med J. 2014;31(7):576-8, doi: 10.1136/emermed-2013-202571.
Ladde JG., Baker S., Rodgers CN., Papa L. The loop technique: a novel incision and drainage technique in the treatment of skin abscesses in a pediatric ED. The American Journal of Emergency Medicine. 2015;33(2):271-6, doi: 10.1016/j.ajem.2014.10.014.
Gottlieb M., Schmitz G., Peksa GD. Comparison of the Loop Technique With Incision and Drainage for Skin and Soft Tissue Abscesses: A Systematic Review and Meta analysis. Acad Emerg Med. 2021;28(3):346- 54, doi: 10.1111/acem.14151.
Gaspari RJ., Resop D., Mendoza M., Kang T., Blehar D. A randomized controlled trial of incision and drainage versus ultrasonographically guided needle aspiration for skin abscesses and the effect of methicillinresistant Staphylococcus aureus. Ann Emerg Med. 2011;57(5):483-491.e1, doi: 10.1016/j.annemergmed.2010.11.021.
Kessler DO., Krantz A., Mojica M. Randomized trial comparing wound packing to no wound packing following incision and drainage of superficial skin abscesses in the pediatric emergency department. Pediatr Emerg Care. 2012;28(6):514-7, doi: 10.1097/PEC.0b013e3182587b20.
Fahimi J., Singh A., Frazee BW. The role of adjunctive antibiotics in the treatment of skin and soft tissue abscesses: a systematic review and metaanalysis. Canadian Journal of Emergency Medicine. 2015;17(4):420-32, doi: 10.1017/cem.2014.52.
Paydar KZ., Hansen SL., Charlebois ED., Harris HW., Young DM. Inappropriate antibiotic use in soft tissue infections. Arch Surg. 2006;141(9):850-4; discussion 855-856, doi: 10.1001/archsurg.141.9.850.
Daum RS., Miller LG., Immergluck L., Fritz S., Creech CB., Young D., et al. A Placebo-Controlled Trial of Antibiotics for Smaller Skin Abscesses. N Engl J Med. 2017;376(26):2545-55, doi: 10.1056/NEJMoa1607033.
Pulia M., Fox B. Antibiotics Should Not Be Routinely Prescribed After Incision and Drainage of Uncomplicated Abscesses. Ann Emerg Med. 2019;73(4):377-8, doi: 10.1016/j.annemergmed.2018.04.026.
Sartelli M., Malangoni MA., May AK., Viale P., Kao LS., Catena F., et al. World Society of Emergency Surgery (WSES) guidelines for management of skin and soft tissue infections. World Journal of Emergency Surgery. 2014;9(1):57, doi: 10.1186/1749-7922-9-57.
Alikhan A., Lynch PJ., Eisen DB. Hidradenitis suppurativa: a comprehensive review. J Am Acad Dermatol. 2009;60(4):539-61; quiz 562-3, doi: 10.1016/j. jaad.2008.11.911.
Humphries AE., Duncan JE. Evaluation and management of pilonidal disease. Surg Clin North Am. 2010;90(1):113-24, Table of Contents, doi:10.1016/j.suc.2009.09.006.
Bojtor AE., Sárdy M., Maródi L. Az elsodleges immunhiánybetegsegek bormanifesztációi. Orv Hetil. 2018;159(23):937-47, doi:10.1556/650.2018.30994.
Rahimian J., Khan R., LaScalea KA. Does nasal colonization or mupirocin treatment affect recurrence of methicillin-resistant Staphylococcus aureus skin and skin structure infections? Infect Control Hosp Epidemiol. 2007;28(12):1415-6, doi: 10.1086/523273.